dinsdag 30 november 2010
1op1 behandelingen
The structure of the department was formed to meet the needs of the population under conditions of confidentiality, including anonymity.
&
All patients are guaranteed confidentiality of information transmitted to them.
(dit lukt dus niet met 5 andere patienten in de kamer)
over lipetsk
Department of Primary Prevention
Department of primary prevention is organized to perform the following tasks:
- Preventing the transmission of diseases, sexually transmitted
- Prevention of diseases and their complications
- Reducing the risk of HIV infection
The Division bases its work on the advocacy and promotion of safer sexual behaviors, coordinating their activities on these issues with NGOs.
Department of primary prevention carries out its work in the following areas:
- Education of sexual culture, promotion of contraception among adolescents and youth, persons with "risky behavior" (prostitutes, homeless people, homosexuals, alcoholics) with active involvement of them in this work;
- Creation of special programs among sanprosvetrabote Not studying and unemployed youth;
- Involvement of NGOs to work with these groups.
Division in their work should include:
- Information on where to get appropriate medical care;
- The assurance that in cases where medical assistance is provided through public / public / services will be provided as the observance of the principles of patient privacy and confidentiality of information;
- Information about what each person should determine their own risk of contracting sexually transmitted diseases through, as well as the risk that affects his / her / sexual partner / partners. If this assessment indicates a high possibility of the disease, this patient shows appeal to the health worker.
the life in russia
- Russians are also big fond of live performances at theatres and since tickets are affordable (prices in cinemas and theatres are comparable), they enjoy attending theatres: opera, musical, ballet, drama etc.
- Movie theatres are also becoming popular in Russia and they are equipped with the latest sound systems.
-The power of an individual in Russia is much less than in the west and most deals are pushed through family, friends and acquaintances. Russian saying is, "One is not a soldier in the battlefield. They often have to rely on their friends to help them out.
Russians believe there is always a roundabout, so they never give up.
-one is supposed to estimate his future income, and pre-pay taxes proceeding from the assumption.
- They don't have a deep respect towards any law, including traffic rules
- Stealing is not considered to be a big deal as long as you have not been caught, and don't steal from your friends or the people you know.
- Russians are used to a situation where everything is unpredictable and unstable.
- Even small things in Russia require much more efforts. Small things that will take you a couple of minutes, in Russia can take you half an hour or even the whole day.
-Russian daily life is tough, and it's probably the reason why they smile so seldom.
- Russian life is built on the base of "God endured, so we have to endure too".
Family life:
- The keyword to Russian family life is dependence. The family life is built on dependence, and Russians are attached to their family members.
- agreeing on casual sex is the way of attracting a partner that she hopes may later offer her commitment.
more:
http://www.ahdaq.com/learning-about-your-russia-love-russian-way-of-life-and-how-to-comprehend-it/
JONGERENVERSLAVING
Jaarlijks geven Russische jongeren zeven miljard dollar uit aan drugs, drank en sigaretten. In totaal drinken ze jaarlijks één miljard liter wodka. Aan drank spenderen Russische jongeren 215 miljard roebel. Ter vergelijking: het jaarlijkse budget van het Russische onderwijs is 80 miljard roebel.
Vooral het aanpakken van het drugsgebruik is moeilijk vanwege het strafrechtelijke verbod op drugs. Vier miljoen Russische jongeren tussen de 11 en 25 jaar gebruiken vaak of minder vaak drugs. Van de jonge druggebruikers rookt 60 procent hasj, 15 procent gebruikt opium en de overigen consumeren heroïne, cocaïne en XTC.
Voor de Russische leerkrachten zijn veertien brochures gemaakt, die hen moeten helpen in het signaleren van drugsgebruik van leerlingen. De brochures hebben een totale oplage van 630.000 exemplaren.
SEKSUELE VOORLICHTING
De bekendste seksuoloog van Rusland, Igor Kon, zegt: 'De gemiddelde leeftijd van het seksuele debuut is in Engeland 16,2 jaar en in Rusland 16,6 jaar. Maar de gevolgen tussen deze debuten bij ons en in Europa vormen een verschil tussen hemel en aarde. Het aantal seksueel overdraagbare aandoeningen en hiv-infecties is onder Russische tieners naar verhouding honderd keer hoger dan in West-Europa. En deze situatie is alleen het gevolg van het feit dat in Rusland seksuele voorlichting op systematische grondslag ontbreekt.
GOKKEN
Moskou telt momenteel 44 casino's, 16.000 automatenzalen en 90 bookmakers. En hun aantal groeit nog steeds snel. Bijna 1,5 miljoen Moskovieten wagen regelmatig een gokje. Er zijn inmiddels 'duizenden' gokverslaafden in de stad.
STADSFOBIEËN
Stedelingen lijden vaak onder aparte stadsangsten. Zo ook de Moskovieten.Gelijkelijk over de geslachten verdeeld (ongeveer een kwart van de fobielijders) zijn ruimtelijke fobieën als pleinvrees, claustrofobie en hoogtevrees. De Moskovieten zijn vooral bang voor elkaar.
BEGRAAFPLAATSEN
Vanwege het groeiende sterftecijfer kampen de begraafplaatsen in Russische steden met plaatsgebrek voor nieuwe graven.
VROUWSOLDATEN
Het aantal vrouwelijke beroepsmilitairen neemt toe in Rusland.
maandag 29 november 2010
Scenario
Evanof uit Levashovo heeft geregeld seks met iemand gehad de afgelopen maanden en hij voelt zich niet lekker. Hij is bang dat hij een soa heeft opgelopen omdat hij onveilige seks heeft gehad. Daarom pakt Evanof de auto naar Sint Petersburg om naar een soa kliniek te gaan. Na een paar uur is hij gearriveerd bij de soa kliniek. Er staan nog een paar andere mensen in de wacht rij, dus het duurt nog even. Als Evanof aan de beurt is gaat hij door de deur naar de doctor. Daar word de doctor geconfronteerd met zijn aandoeningen. De doctor neemt een bloed sample af om te laten testen. Na het afnemen van een sample krijgt hij de aidkit mee uit handen van de doctor. Evanof neemt de aidkit mee naar huis. Na een paar uur rijden is hij dan eindelijk thuis en ziet iets opvallends aan de aidkit. Hij word nieuwsgierig en interacteert op de een of andere manier mee waarbij informatie word gegeven over risicovol seks gedrag. Tevens word hij niet geconfronteerd met feiten die er voor kunnen zorgen dat hij angstig afwacht op zijn test resultaten. Als Evanof na een week terug komt bij de kliniek is het moment van de waarheid in zicht. De doctor heeft geen sporen van soa's gevonden maar wel andere virussen. Na afloop van het gesprek vraagt de doctor over de aidkit. Of Evanof iets geleerd heeft of dat het enig effect op hem heeft gehad.
Media strategie: verslag
conclusies: samenvatting van de bevindingen!
- kansen
Verdeling:
Situatie-analyse regio = inleiding probleem rusland!
Probleemstelling = Ans
Media-landschap = Nermin
Omgeving community =steven
Bevolkingskarakteristiek = dion
Strategische opties/scenario’s=remco
Strategie
specifiek probleem oplost. Aangezien er sprake is van 'mediastrategie' zou
je eraan toe kunnen voegen: middels de inzet en toepassing van media
(nieuwe, zowel als traditionele).
Daarbij zou elke door jou genoemde dimensie van toepassing kunnen zijn.
Waarbij je, afhankelijk van het gebied en de mensen, vaak niet moet denken
in 'communicatiestrategieen' zoals wij ze vandaag de dag hier in het Westen
toepassen, maar veel meer basic. Denk bijv. nog even aan het voorbeeldje van
Sandra tijdens de Kick-Off: een soort van pictogrammenspel rondom het
HIV-probleem. Kortom: alles wat communiceert c.q. kan communiceren is in
principe een medium.
Van belang is dan ook - wil je een goede, effectieve mediastrategie kunnen
ontwikkelen - dat je een concreet, duidelijk en relevant 'probleem' hebt
geformuleerd. Anders blijf je zweven.
Kijk nog even naar de opdrachtformulering in de modulebeschrijving, ik heb
geprobeerd het daar zo concreet/realistisch (en behapbaar!!) mogelijk neer
te zetten.
quotes voor doel
“In addition, interventions targeted to Russian men to promote condom acceptance, reduce domestic violence, and increase awareness of the increasing dangers of HIV also will have a positive impact on women in Russia”
“One challenge facing educational efforts in Russia is that many citizens report substantial mistrust of media and government information sources. More than half of our participants were skeptical that the government and Russian media could be trusted to provide accurate information concerning HIV. Establishing trust with relevant, vulnerable populations is a cornerstone of good clinical and public health practice and will be an especially important component of HIV prevention interventions for this population.”
“Interventions designed to promote knowledge and increase awareness about HIV are the among the most realistic sustainable interventions for a country with modest resources and in the midst of dramatic social change”
“The Information–Motivation–Behavioral Skills (IMB) model asserts that individuals engage in AIDS preventive behavior when they have accurate information regarding the disease, are sufficiently motivated to avoid it, and have skills adequate to implement healthy behaviors (Fisher & Fisher, 1992)”
Doelgroep STD/STI
Demografic

a thorough review of the scientific literature uncovered no studies that specifically evaluated the HIV-related knowledge and attitudes of men and women attending Russian STD clinics. Because of the potential for this group to be severely affected by the burgeoning HIV epidemic in Russia and to serve as a core transmitter group facilitating the wider dissemination of HIV, a thorough characterization of the knowledge, sources of HIV/AIDS information, attitudes, and beliefs of this group is warranted in preparation for the development of behavioral risk reduction interventions to help stem the further spread of HIV in Russia.
Because condoms are relatively expensive in Russia, and because high-quality condoms are difficult to obtain (Lunina and Lunin, 1994; Meade et al., 1998), we expected to find substantial variation in attitudes toward condom use in Russia as compared with the United States and other Western countries.
The St. Petersburg Municipal Skin–Venereal Dispensary is the largest STD clinic in St. Petersburg, Russia’s second largest city. The clinic sees nearly 200,000 outpatients each year and also maintains 150 inpatient beds. The clinic is funded by the municipal government of the city of St. Petersburg and provides both free services and paid for services.
Over two-thirds of respondents had obtained HIV/AIDS-related information from each of the three media sources (89.6% from a magazine or news- paper article, 80.4% from television, and 67.0% from radio). Fewer respondents (61.6%) had talked with family and friends about HIV/AIDS and only 20.1% had heard about HIV/AIDS from a teacher
Women reported significantly more sources of information than did men. The number of sources decreased steadily with increasing age
Most respondents (71.3%) said that they would like to learn more about HIV and AIDS. A large majority reported that they believe the government and the media are not telling the truth about AIDS (68.4% and 62.5%, respectively). Only 10.7% of the sample personally knew someone with HIV or AIDS.
Women’s knowledge scores were significantly greater than men’s
Knowledge scores steadily increased with increasing educational attainment, and decreased with in- creasing age for participants older than 18 years of age.
Participants who said they believe that the government is telling the truth about AIDS, and those who believe the media are telling the truth, scored higher on the knowledge scale than did respondents who distrusted the government, the media, or both.
Also, participants who wanted to learn more about HIV/AIDS had higher knowledge scores than those who did not want to learn more
However, there was no difference in knowledge between respondents who knew someone with HIV/AIDS and those who did not.
Condom Attitudes

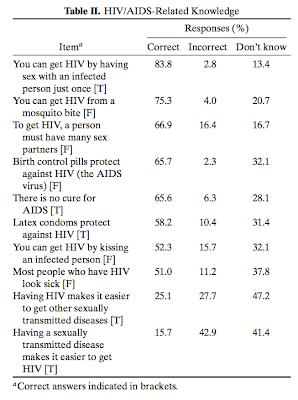
Members of this high-risk population showed significant deficits in HIV transmission knowledge, with a mean score of 55% correct on the HIV/AIDS knowledge test.
Nearly half of the participants in this study did not know that HIV cannot be transmitted through kissing, almost one fourth did not know that it cannot be transmitted by mosquitoes, and more than one third did not know that oral contraceptives offer no protection against HIV.
In this sample of STD clinic clients, the women were more knowledgeable and re- ported more sources of HIV/AIDS information than the men, suggesting that Russian women may be more likely than their male counterparts to seek out HIV/AIDS information from multiple sources.
Also, younger respondents reported greater numbers of sources of HIV/AIDS information and demonstrated greater HIV/AIDS knowledge.
greater knowledge was associated with younger age, higher educational attainment, positive attitudes to- ward condoms, having more sources of information about HIV/AIDS, and believing that the government is telling the truth about AIDS.
One challenge facing educational efforts in Russia is that many citizens report substantial mistrust of media and government information sources. More than half of our participants were skeptical that the government and Russian media could be trusted to provide accurate information concerning HIV. Establishing trust with relevant, vulnerable populations is a cornerstone of good clinical and public health practice and will be an especially important component of HIV prevention interventions for this population.
Interventions designed to promote knowledge and increase awareness about HIV are the among the most realistic sustainable interventions for a country with modest resources and in the midst of dramatic social change (Kalichman et al., 2000; Kelly and Amirkhanian, 2003)
Artikel 2: HIV Risk Behavior in Male and Female Russian Sexually Transmitted
Disease Clinic Patients (artikel van Nermin)
Inleiding/conclusies (door de auteurs)
Alcohol use in
conjunction with sexual activity was common in this sample (85%)
One-third of study participants had more than 1 partner in the past 3 months, and about half (48%) of the sample had previously been diagnosed with an STD. However, despite this evidence of high-risk behavior, most participants (67%) reported using condoms less than half the time.
our research has documented low perceptions of vulnerability among at-risk groups in Eastern Europe, poor understanding of how the virus is transmitted, and low acceptance of protective measures such as condom use or limiting the number of sexual partners
Future risk reduction intervention
efforts for this group must be grounded in a solid understanding of the factors associated with risky behaviors
High-risk behavior was associated with substance use and lower perceived severity of AIDS. Self-protective strategies differed by gender: men reported higher condom use rates whereas women reported efforts to limit their number of sexual partners
Resultaten
Demographic Characteristics
For the 400 participants, the mean age was 29.4 years (SD = 10.6), with a range of 14 to 64 years old.
Participants reported a median monthly income of 2000 rubles, less than half of the median Russian
monthly income of 5600 rubles
Forty percent reported at least some university- level education.
The majority of participants (57.8%) reported that they currently were single, but a substantial number reported that they were married (31.9%) or living with someone (10.3%).
Almost half of the sample (48%) reported a past history of STDs, with the most frequent being chlamydia(24%), gonorrhea (19%), syphilis (18%), and herpes (5%)
Six participants (1.5%) reported that they were HIV-positive. Thirteen percent of the sample reported a history of multiple lifetime STDs. past history of STDs reported more lifetime sexual partners and lower rates of condom use
Perceived Severity of HIV/AIDS
The substantial majority of participants perceived AIDS as severe; 78% indicated that being diagnosed with AIDS was the worst thing that could happen to them. Men reported significantly lower perceptions
of the severity of AIDS than women
Perceived Vulnerability/Worry About
Contracting HIV/AIDS
31% “not at all”,
35% “little worried
22% “somewhat worried
12% “very worried”
Our work has found that many Russian citizens continue to believe themselves insulated from the epidemic, and therefore do not believe it is important to take measures to protect themselves
Five percent of the men and none of the women reported
same sex partners during their lifetime.
Condom Use During Sexual Activity
18% “never”
49% “some of the time”
12% “half of the time”
21% “most or all of the time”
Male STD clinic patients were more likely than female patients to report that a condom was used during their most recent sexual intercourse act, 63% versus 48%
Participants who reported that their sexual partners regularly used alcohol in conjunction with sexual activity were less likely to use a condom during their most recent sexual encounter.
Participants who perceived AIDS as more severe also were more likely
to use a condom during their last sexual act
Multiple Sexual Partners During 3 months
33% of the sample reported multiple sexual partners
during the previous 3 months, with a mean of 1.87 partners
men 42%
women 24%
single individuals 52%
married 24%
men with men 88%
Having multiple sexual partners was significantly associated with personal alcohol use in conjunction with sexual activity
Having multiple partners also was associated with lower perceived severity of AIDS
One positive finding was that participants reporting multiple sexual partners reported higher rates of condom use than participants not having multiple sexual partners
Strategies to Avoid HIV in the future (suggested by participants)
61% “use condoms”
50% “fewer sex partners”
43% “choose partner more carefully”
42% “have sex only with a main partner”
9% “staying abstinent”
Individuals who were more worried about contracting HIV endorsed more future strategies to avoid the virus
Discussion
Russian STD clinic patients in this study reported relatively high rates of HIV risk behavior, including
having multiple sexual partners over the previous 3 months, consuming alcohol in conjunction with sexual
activity, and low condom use rates. Almost half of the patients had experienced a past STD, yet only 21% reported protecting themselves with consistent condom use.
Marital Status, Monogamy,
and HIV Risk
One surprising finding of this study was the substantial number of participants who reported being married or living with a long-term partner (42%). This number is much higher than the percent of married or partnered individuals reported in published studies of American STD clinic patients (10–28%)
only 47% of married/partnered individuals indicated that they would reduce their risk
for HIV in the future by limiting themselves to having sex only with their primary partner.
Mutual monogamy between two healthy individuals is an effective disease- prevention strategy, but does not appear to be a goal of a substantial percentage of this high-risk sample. (9%)
In this sample of Russian STD clinic patients, 5% of the men and none of the women reported same-sex sexual contact.
Weinig sex workers en drug users:
2 women (1%) and 4 men (2%) reported 10 or more sexual partners in the previous 3 months, suggesting the possibility that these individuals were engaging in formal commercial sex work.
17% of participants reported such use and 15% indicated that their sex partners used illicit drugs in conjunction with sex.
Prevention models developed in the United States frequently rely upon negotiating condom use with partners, sexual assertiveness skills, and refusing to engage in unsafe activities. Such approaches may not be safe
and practical for Russian women. Domestic abuse and violence toward women in Russia is a pervasive problem (Horne, 1999). Women who insist upon condom use with a long-standing sexual partner may be placing themselves at risk for assault and may raise suspicions regarding their own fidelity. Russian women are taking another route to reduce their risk for disease. Reducing the number of sexual partners can be an effective means of disease prevention, but only if these partners are also sexually monogamous, a condition that does not appear to be widespread in this sample.
!!!In addition, interventions targeted to Russian men to promote condom acceptance,
reduce domestic violence, and increase awareness of the increasing dangers of HIV also will have a positive impact on women in Russia.!!!
The Information–Motivation–Behavioral Skills (IMB) model asserts that individuals engage in AIDS preventive behavior when they have accurate information regarding the disease, are sufficiently motivated to avoid it, and have skills adequate to implement healthy behaviors (Fisher & Fisher, 1992).
The IMB model also addresses the importance of motivation to engage in HIV preventive behaviors. The relatively low perceived vulnerability to HIV in the sample is notable given that these individuals were
presenting for STD testing and treatment at the time of the survey. Simply increasing patient knowledge about the heightened risk of HIV in Russia may serve to motivate some individuals to engage in protective behavior.
Artikel 3: COMPARISON OF HIV/AIDS KNOWLEDGE AND ATTITUDES OF STD CLINIC CLIENTS IN ST. PETERSBURG, RUSSIA AND MILWAUKEE, WI, USA (samenvatting is van vorige week)
Parallel surveys were conducted at the St. Petersburg Municipal Skin-Venereal Dispensary and the Milwaukee Central Health Clinic. At each clinic, consecutive samples of 200 men and 200 (St. Petersburg) or 201 (Milwaukee, WI) women were asked to complete self-administered questionnaires regarding their personal characteristics and HIV-relevant knowledge, attitudes, and behavior. Although not every participant answered every question, no one refused to participate.
The St. Petersburg Municipal Skin-Venereal Dispensary is the larg- est STD clinic in St. Petersburg, which is Russia’s second largest city with a metropolitan population of approximately 5 million people. The clinic serves nearly 200,000 outpatients each year. The clinic is funded by the municipal government of the City of St. Petersburg, and provides both free services and paid-for-services.
Six Russians (1.5%) reported that they were HIV-positive.



Conclusions:
nterventions for Russian and American STD clinic patients may well take different forms. Russian patients in particular appear to need information-based and awareness raising approaches and also may benefit from efforts to provide at-risk individuals with a more accurate understanding of their vulnerability to HIV. Media campaigns, peer interventions, and school-based informational approaches in Russia would seem appropriate to more widely disseminate the facts concerning HIV/AIDS.
Both American and Russian STD clinic patients have difficulty trusting government and media sources of information regarding HIV. These patients may place greater trust in their health care providers than in (apparently) suspect govern- mental sources of information. Service providers should take advantage of the opportunity to educate patients, heighten their awareness of HIV, and advocate for testing.
COMPARISON OF HIV/AIDS KNOWLEDGE AND ATTITUDES OF STD CLINIC CLIENTS IN ST. PETERSBURG, RUSSIA AND MILWAUKEE, WI, USA
Municipal Venereal Diseases Dispensary
Городской кожно-венерологический диспансер
een website met een overzicht van alle klinieken in st petersburg
STI kliniek lipetsk
STD clinic
http://www.springerlink.com/content/pt117u655201271j/
procedure std clinic GENERAL
Many STI clinics offer free, confidential STI and HIV testing. Some clinics will see clients on a drop-in basis, although appointments are recommended. Treatment, prescriptions or immunizations may be given, and referrals can be made to appropriate specialists. Information on STIs and HIV, safer sex, and risk reduction is available. The clinic staff is happy to discuss any questions you may have regarding sexual health. Free condoms are usually offered.
Diagnosis and Treatment of Infections
Clinics focus on the diagnosis and treatment of STIs. They are not family planning clinics - birth control is not offered. Routine Pap smears are not done routinely at a clinic, and women still need to have these done through a family physician.
A routine visit would include tests for:
Chlamydia
Gonorrhea
Syphilis
Candidiasis/yeast (females)
Trichomoniasis (females)
Bacterial vaginosis (females)
HIV tests are done on request
After taking your history, the nurse may recommend other tests for:
Hepatitis A
Hepatitis B
Hepatitis C
Non-gonococcal urethritis (males)
Herpes Simplex
Some STIs are diagnosed by examination only. These include:
Yeast balanitis (males)
Genital warts
Molluscum contagiosum
Pubic lice
Scabies
Non-STI rashes and skin conditions affecting the genitals
Other Services
Some clinics offer Hepatitis vaccinations as a part of STI care. Others may include a needle exchange.
What should I expect at the clinic?
An STI clinic provides free, confidential testing and diagnosis for STIs and HIV, and treatment for most STIs.
Consultation
The health care provider will call you, and take you to an examination room. After discussing the reason for your visit, the health care provider will ask questions about any symptoms you may be experiencing, as well as assess your risk for STIs. This involves personal questions about your sexual history, sexual partner(s), and practices including condom and drug use. These are necessary to determine exactly which tests should be done. Yourconfidentiality and privacy will be protected.
1. Examination and Swab Tests
After your history is taken, the health care provider does a genital examination. Some STIs can only be diagnosed this way. The health care provider will examine your skin in general, and more specifically, the area around your genitals.
For women, the examination is similar to having a Pap smear. You lie on the examination table, unclothed below the waist and covered with a paper sheet, and your feet rest in special supports with the legs apart. When you are comfortable, the health care provider checks the lymph nodes in your groin and examines the external genitals with gloved hands and a cotton swab. An instrument called a speculum is used to hold the walls of the vagina apart to view the cervix. The speculum is shaped a bit like a duck bill and is about the size of 2 outstretched fingers. The speculum is lubricated with water and is slowly inserted into the vagina and opened slightly. Insertion of the speculum should not be painful if the vagina is relaxed. The usual sensation is a slight pressure as the vaginal walls are held apart.
The health care provider takes swabs for chlamydia and gonorrhea from the cervix, and swabs from the vaginal walls for yeast, bacterial vaginosis and trichomoniasis. A Pap test may be included. After the swabs, the speculum is removed. The health care provider then will do an examination by hand, which involves placing 2 gloved and lubricated fingers inside the vagina and feeling the abdomen on the outside with the other hand. This helps the health care provider determine whether there is any tenderness or abnormal masses in the pelvic area.
The examination for men is simpler. A man lowers his pants and underwear to mid-thigh, and the health care provider examines the genitals and pubic region with the man standing at the foot of the examination table. The health care provider checks the lymph nodes in your groin as well as feels the testicles for lumps or discomfort.
It is important that men do not urinate for 2 hours prior to an STI exam.
Most men are then sent for a urine specimen to test for gonorrhea and chlamydia. If a man is experiencing symptoms highly suggestive of either of these infections, or has come in because a sex partner has them, a urethral swab is done before the urine test. This involves inserting a thin swab a short distance into the urethra and gently rotating it to collect any organisms or inflammatory cells. This test is uncomfortable, but lasts only a few seconds. There may be some discomfort for a short time afterwards, especially when urinating (a slight burning sensation).
2. Blood Tests
Some infections are tested through blood tests. These include HIV, syphilis and hepatitis.
Results
Some results may be ready before you leave, others will be available in one week. With the exception of HIV, all test results are available over the telephone. HIV results must be given in person.
Treatment
If the examination or tests indicate an infection, treatment may be started on the same day. Treatments for reportable STIs - chlamydia, gonorrhea, syphilis - are provided free of charge, as is liquid nitrogen treatment for genital warts. Over-the-counter medications may be suggested for some conditions, and prescriptions may be available for initial herpes outbreaks. Hepatitis vaccinations may be offered to clients at risk.
STI Information
You are encouraged to ask questions about STIs, safer sex, and sexual health. This site and our information phone line also have information about these issues.
Confidentiality
Information that you give to a health care provider and the results of any tests you have, are confidential. Some STIs (chlamydia, gonorrhea, syphilis) are reportable, which means that you and your sexual partners are required to receive treatment.
(is dit in rusland wel zo???!)
zondag 28 november 2010
Alternatieve klinieken?
Zoeken
Soa-klinieken Russia?
http://www.soaaidsmagazine.nl/artikel_internationaal/295
Sanam kliniek: PTT
http://www.authorstream.com/Presentation/Belly-14514-Ausheva-Women-HIV-social-economic-driving-forces-epidemic-Russia-Current-conditions-Societal-polit-notes-Science-Technology-ppt-powerpoint/
Idéale procédure bij SOA/HIV-onderzoek
Idéale procédure bij SOA/HIV-onderzoek:
Je kan kiezen tussen:
1. een soa-onderzoek inclusief hiv-test
2. een soa-onderzoek exclusief hiv-test
3. alleen een hiv-test
Hoe verloopt een SOA-onderzoek:
Gesprek:
- krachten
- manier van vrijen
Lichamelijke onderzoek:
- op basis van de antwoorden krijg je een lichamelijke onderzoek
- voor de onderzoek word er precies uitlegt wat er zal worden onderzoekt
- hoe je de soa- uitslag krijgt
Het onderzoek:
- symptonen van soa
- "materiaal" zal op verschillende plaatsen worden verzameld:
- uitstrijkjes
- urine
- of sommige gevallen bloed
Laboratorium onderzoek= spreekt voor zich!
Uitslag:
- twee week tot uitslag (soa/hiv test)
- bij HIV test wordt gevraagd om persoonlijk lang te komen voor de uitslag
- Bij Soa kan de uitslag telefonische worden medegedeeld
- Als je HIV positief bent, krijg je begeleiding en informatie, behandeling
- Bij Soa's wordt ook gewoon behandeld
Je moet voor een HIV- test van te voren zelf toestemming geven







